Long waiting lists in NZ's public health system: Causes and impacts on patients
Long FSA and surgery waiting lists in NZ’s public health system mean Kiwi patients face dire situations with grim outcomes. Know how health insurance can help.
Wait times for medical assessment, surgery, and other treatments are a nightmare for thousands of Kiwi patients, taking a massive toll on them and their loved ones - physically, emotionally, and financially.
The figures below give an alarming insight into the dilemma facing New Zealand’s public health system.
- In June 2023, over 51,000 patients waited 4+ months for their first specialist assessment (FSA). By February 2025, this number had jumped to more than 74,000.
- From March 2024 to February 2025, the number of patients waiting longer than 4 months for treatment ranged between 27,000+ and 37,000+.
- In September 2023, more than 3,900 patients were waiting more than 1 year for treatment.
There is only one realistic way to protect yourself and your family from suffering the impacts of a strained public health system: private health insurance. As of mid-2024, nearly 25% of doctors in New Zealand are working exclusively in the private sector, while roughly 12% are working both in public hospitals and the private sector. Medical insurance allows you to access more doctors and facilities without worrying about the costs of private healthcare.
Important caveat: Medical insurance plans are not created equal. Some focus on everyday healthcare needs, while others offer comprehensive protection. Policywise’s insurance experts can help you compare plans from New Zealand’s best health insurers and choose the right solution for your needs and budget.

Learn more about different types of insurance from a licenced financial adviser and see what's best for your circumstances.
nib | Accuro | Southern Cross | Partners Life | AIA

Learn more about different types of insurance from a licenced financial adviser and see what's best for your circumstances.
Health | Life | Trauma | Total and Permanent Disability | Income Protection

Source: Ministry of Health
Factors contributing to long wait times in the New Zealand public health system
Long wait times for first specialist assessments and treatments have been an issue in New Zealand even before the Covid-19 pandemic overstretched the health system. In January 2019 (prior to the first identified Covid-19 case), over 10,000 Kiwi patients were waiting longer than four months for their FSA.
Even so, Covid-19 added huge pressure. As the country stepped up its fight against the pandemic, other healthcare services were derailed. Many outpatient appointments and treatments, including elective surgeries, had to be deferred during lockdowns. Diagnostic scans, including MRIs, mammograms, and colonoscopies, were postponed or delayed.
The number of patients waiting more than four months for treatment tripled - from over 4,300 in January 2019 to 11,900+ by January 2021 (almost a year after the country’s first Covid-19 case), then to almost 33,000 by January 2022.
As of January 2025, over 37,000 patients have been waiting more than the target period for their treatment and over 77,000 patients have been waiting 4+ months for their FSA.

Source: Response to OIA Request (May 2024); Ministry of Health
Several long-standing, growing concerns – such as insufficient funding and workforce shortages – were aggravated by Covid-19, compounded burnout, and low morale among the country’s medical professionals.
Lack of funding
New Zealand’s core health expenditure has lingered below 7% of GDP since at least 2010, while comparable countries are averaging 12%. Budget allocation for public healthcare cannot keep up with demand and inflation. Health New Zealand Te Whatu Ora is requesting immediate strategies be put in place to manage budget deficits and staffing shortages.
These budgetary constraints may impact patient care and how quickly staffing shortages are filled. They may also restrict or delay investments in maintaining and modernising public health facilities, increasing hospital beds, and purchasing vital medical equipment.
Health workforce shortages
New Zealand has an acute shortage of health professionals. Data released by Health New Zealand Te Whatu Ora in July 2023 estimated the shortages at 1,700 doctors (including GPs), 4,800 nurses, 1,050 midwives, 220 oral health practitioners, and 200 anaesthetic technicians, among others.
A member survey by the Association of Salaried Medical Specialists (ASMS) revealed that remuneration, workloads, and tight workplace conditions had driven many health professionals to consider opportunities outside the public health system. Some intended to emigrate, while others opted to stay in the country but focus on private practice. This strained staffing situation is expected to worsen over the next decade as healthcare demands increase, lengthening patient wait lists even more.

Source: Health New Zealand | Te Whatu Ora
Aside from contributing to ballooning wait lists, the shortage of GPs and medical specialists also means that some areas don’t even have physicians, forcing patients and their families to travel up to 100 km just to see a doctor.
Burnout and low morale among health professionals
Long waiting lists that lead to delayed diagnoses and patient care have multiple implications. Patients' conditions worsen and healthcare resources are further drained to provide them with care at the latter stages of their disease. Overwhelmed medical professionals are frustrated in providing the timely treatment and quality of care their patients need.
These challenging situations add to the pressure on many healthcare workers. In fact, surveys by ASMS found that work-related burnout remained high among senior medical and dental specialists. In the 2015 and 2020 surveys, 42% and 44% of respondents were experiencing work-related burnout. Respondents attributed this to workload pressures, long hours, resource constraints, Covid-19, and frustration with management and the system.
Ageing population
With nearly 17% of New Zealand’s population classified as ageing (estimated to rise to 24% or around 1.5 million over the next 30 years), demand for elective surgery - such as joint replacements, long-term care for age-related chronic conditions, and other services in public hospitals - is on the up. Kiwis in the public healthcare sector are feeling the stress as more elderly patients wait too long to see a specialist and receive the treatment they need.
How long are our waiting lists? A closer look at assessment and treatment delays
With New Zealand’s public health system in crisis, the delivery of prompt, high-quality medical care to needy patients is at breaking point.
The long wait to see a specialist
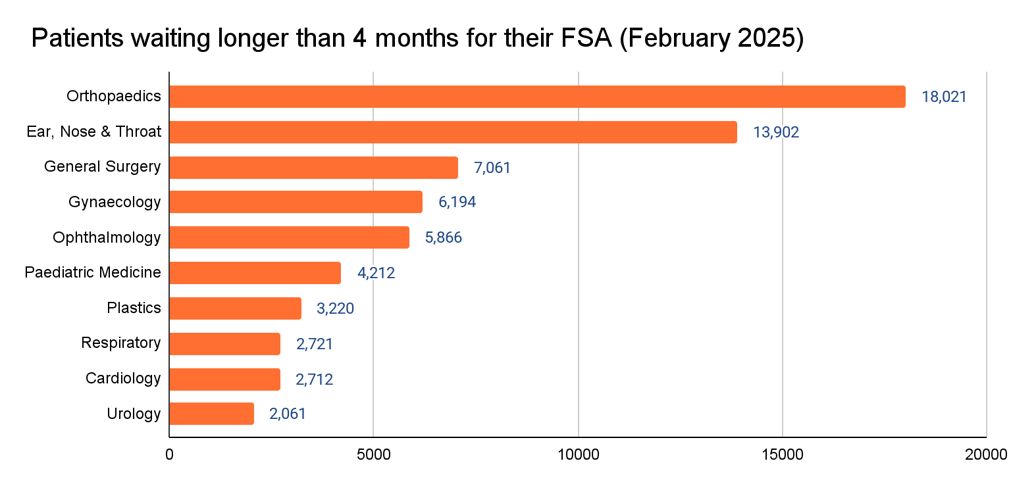
Patients accepted for first specialist assessments (FSAs) should be seen within four months from their referral date. But as of February 2025, over 74,000 patients had been waiting longer than that for their FSA. Ten specialities had over 2,000 patients waiting longer than four months.
Specialities with the highest number of patients with delayed FSAs were:
- Orthopaedics (18,021)
- Ear, nose & throat (13,902)
- General surgery (7,061)
- Gynaecology (6,194)
- Ophthalmology (5,866)
- Paediatric medicine (4,212)
- Plastics (3,220)
- Respiratory (2,721)
- Cardiology (2,712)
- Urology (2,061).
Source: Ministry of Health
Treatment delays
Patients given a commitment to receive treatment should receive it within four months. As of February 2025, over 36,000 patients have been waiting more than four months for treatment.
Specialties with the highest number of patients with delayed treatments were:
- Orthopaedics (8,469)
- Ophthalmology (6,055)
- Ear, Nose & Throat (5,240)
- General Surgery (4,349)
- Dental (3,573)
- Gynaecology (2,973).

Source: Ministry of Health
Orthopaedics, ophthalmology, ENT, general surgery, dental, and gynaecology recorded the highest number of treatment delays from March 2024 to February 2025.

Source: Ministry of Health
Several paediatric surgery patients also waited longer than target wait times for first specialist assessments and treatment.

Source: Ministry of Health
Health New Zealand Te Whatu Ora’s December 2023 Clinical Performance Metrics report revealed that by the end of September 2023, more than 3,900 patients had been waiting more than a year for treatment.

Source: Health New Zealand | Te Whatu Ora. Clinical Performance Metrics - July to September 2023; Note: Data for Taranaki requires further validation.
RECOMMENDED READINGS
Non-Pharmac drugs: What they cost & how health insurance can help
Cost of private surgery in New Zealand
What ACC does not cover and how to fill the gap
Comparing health insurance in NZ: 2025 buying guide & quotes
Medical insurance for pre-existing conditions
Getting health insurance for your family
The disturbing impact of long wait times on patients and their families
Deteriorating health and quality of life
Assessment and treatment delays prolong patients’ suffering. In some cases, their condition worsens to a point where they require more complex procedures, or treatment can no longer save them.
The uncertainty and constant pain add to patients’ mental anguish, with some developing anxiety and depression as they wait to receive the help they need. Many cannot perform everyday tasks and are forced to rely on others.
This ordeal is also difficult for patients’ loved ones. Partners, family members, and friends often struggle to find ways to reduce the patient’s suffering and decide to take time off work to care for them, support them financially, and raise funds for private healthcare expenses.
A Canterbury woman in her 50s was on several medications to manage the “debilitating pain” caused by her “crumbling right hip.” Her doctors, who knew she needed a hip replacement, had been referring her for an FSA since 2018. But the referrals kept getting rejected.
She was forced to use a walking stick to move around and needed the help of friends to care for over 40 animals. She continued working part-time, but life became increasingly difficult and the drugs she was taking couldn’t take the pain away completely. As such, she struggled to sleep: "I haven't had a decent sleep in two years. There is no quality of life."
Her friends put her on suicide watch several times as they knew how upset she was: “You can't keep taking all these drugs and be on top of the world all the time.”
In September 2019, her orthopaedic surgeon requested an urgent assessment from the DHB (now Health New Zealand Te Whatu Ora). She was finally accepted onto the list and her FSA was scheduled for February 2020.
Mounting financial burdens
Patients on long waiting lists suffer declining health, often developing severe issues that need more advanced treatments, costing the public health system more resources.
Treatment delays can also affect patients’ capacity to support themselves and their loved ones. Some continue working despite their deteriorating health, while others are forced to work part-time. Others have to take extended time off work, as might their families, thus losing income when they need it most.
Back surgery for a Taranaki mother was cancelled three times due to bed shortages. A severe sciatic nerve issue meant she had to take medications to ease the pain. Worried about the pain meds’ addictive effects, she tried skipping them, only to end up crying in agony.
Her mother and sister took annual leave three times to help look after her and her children. Her husband eventually stopped working to care for her as she needed help with mobility, getting out of bed, and showering.
Before this, the mother of three had struggled to even get into the public health system. In 2021, her GP’s specialist referrals were rejected four times as her case was not deemed urgent. In January 2022, she finally had an MRI. During her appointment with a specialist, she was told she needed surgery.
As of July 2022, she still hadn’t had her surgery, and when booked for September 2022, was told there was no guarantee it would happen.
Health insurance as a valuable escape from long wait times
In many medical cases, time is of the essence. Waiting too long for diagnosis and treatment can mean prolonged suffering, worsening health, and lost income for patients and their families. For others, such delays can narrow the gap between life and death and, in terminal cases, rob patients of more precious time they could have spent with loved ones.
For patients struggling with the cost and impact of long wait lists, private health insurance can be a literal lifeline. Providing faster access to care and financial support for treatments not covered by the public system, private health insurance offers a much-needed and vital alternative.
Medical insurance gives patients the option to use private health facilities where they can be screened and treated faster. On top of speedier access to appropriate healthcare services, having the right private health insurance plan eases the financial burden of serious illnesses, lightening the cost of specialist consultations, diagnostic tests, procedures, and surgeries. Some medical insurance plans even pay for costly life-saving and life-extending treatments not covered by Pharmac. Medical choices are not limited by what patients and families can afford, nor do they need to sell off properties or get into debt to receive timely care.
Blair Vining was diagnosed with terminal bowel cancer at 38 and initially given six to eight weeks to live. After receiving a letter saying he couldn’t be seen by an oncologist for eight to ten weeks, Blair and his wife decided to go private. After three weeks, he was able to start his treatment.
Shortly after, Blair’s bowel became obstructed and he needed surgery fast. Unable to find available doctors in Invercargill and Dunedin to perform the procedure, he had to be flown to Christchurch Hospital.
But wait times and doctors’ availability weren’t the only obstacles. Blair’s treatment involved an unfunded drug (Cetuximab) which, at the time, cost $30,000 a month. The same drug is publicly funded in Australia.
When Blair realised that other cancer patients also struggled with long wait times and accessing better treatment, he started gathering signatures to petition for the creation of a national cancer agency.
Blair’s family also helped declined patients access private colonoscopies in the hope that an early diagnosis would give them a better chance of beating cancer. His wife, Melissa, together with many volunteers, donors, and partners, worked to open the Southland Charity Hospital. The hospital provides free colonoscopies (amongst other procedures) to Otago and Southland residents who can’t get onto the public health waiting list or afford private healthcare.
Blair passed away in October 2019, after fighting for changes in the public health system and inspiring movements to provide better cancer care.
Policywise: Helping you find the right health insurance plan for your needs
Policywise is a 100% free service which tells you which medical insurance plan best fits your needs. We offer fast, comprehensive, and easy-to-understand comparisons of all leading providers, and a simple summary clearly recommending which insurer is best for your situation.
Not all insurance policies are the same. Policywise can help you sort out the duds, avoid the lemons, understand the fine print and exclusions, and get the right insurance for you and your family.
We make the important decision of where to buy your insurance super easy. We’ll answer your questions, provide experienced advice and quotes, and manage all the back and forth throughout the application process. Taking out your cover through us means you'll have our lifetime support and claims advocacy, and we'll help you negotiate a positive outcome at claim time. We can also take care of lodging any claims on your behalf and back you up if the going gets tough.
Check out the reviews on our homepage for how other New Zealanders have found our service because now is the time to get your health insurance sorted. Give your family or someone you love the most outstanding financial support possible. Book a 5-minute callback with Policywise today; our service is fast and free.
Important Disclaimer: The information on this website is general in nature and does not consider your personal situation. It is not intended as a definitive financial guide. Before making any KiwiSaver or insurance decisions, we recommend speaking with a licensed Policywise adviser.
Policywise advisers are licensed by the Financial Markets Authority to give financial advice on KiwiSaver and health, life, and disability insurance. For more, see our Public Disclosure page.
All insurance is subject to insurer approval. Policies may include stand-down periods, exclusions, terms and conditions, and premium loadings not listed here. Optional (add-on) benefits come at an extra cost. Please refer to the relevant policy document for full and current details, as insurers may update these at any time.
Product pages on this site are summaries only. In the case of any difference between website content and the provider’s official policy wording, the provider’s wording will apply.
Quickly find the cover that’s best for you
Policywise tells you which health, life or disability insurance best matches your circumstances, 100% free. Talk to one of our insurance advisers to find out which health or life insurance is best for you.
Readings and references
Association of Salaried Medical Specialists. (2019). Hospitals on the Edge. Retrieved 22/05/2023 https://asms.org.nz/wp-content/uploads/2022/05/Hospitals-on-the-Edge.pdf
Association of Salaried Medical Specialists. (2020). Building the workforce pipeline, stopping the drain. Retrieved 22/05/2024 https://issuu.com/associationofsalariedmedicalspecialists/docs/building_the_workforce_pipeline__stopping_the_drai
Association of Salaried Medical Specialists. (2021). The moral injury of keeping patients waiting. Retrieved 09/04/2023 https://asms.org.nz/the-moral-injury-of-keeping-patients-waiting/
Association of Salaried Medical Specialists. (2023). A Less Public Place. Retrieved 22/05/2024 https://asms.org.nz/wp-content/uploads/2023/08/A-Less-Public-Place-FINAL-1.0.pdf
Association of Salaried Medical Specialists. (2024). Anatomy of a health crisis. Retrieved 22/05/2023 https://asms.org.nz/wp-content/uploads/2024/04/ASMS-Anatomy-of-a-Health-Crisis-210416.pdf
Health NZ Te Whatu Ora. (2022). How is my DHB performing? Retrieved 20/04/2023 https://www.health.govt.nz/new-zealand-health-system/health-targets/how-my-dhb-performing
Health NZ Te Whatu Ora. (2023, December 19). Clinical Performance Metrics - July to September 2023. Retrieved 28/04/2025 https://www.tewhatuora.govt.nz/publications/clinical-performance-metrics-july-sept-2023
Health NZ Te Whatu Ora. (2024). Faster Cancer Treatment and Shorter Stays in Emergency Department. Retrieved 19/04/2023 https://www.health.govt.nz/new-zealand-health-system/accountability-and-funding/planning-and-performance-data/faster-cancer-treatment-and-shorter-stays-emergency-department
Health NZ Te Whatu Ora. (2024). Request for official information, reference: HNZ00042929: Number who have been waiting for FSA for > 4 months [Unpublished data]
Health NZ Te Whatu Ora. (2025, January 22). Request for official information, reference: HNZ00072666: Headcount and full-time equivalent (FTEs) of doctors working for public hospitals vs private, for up to three worksites (1 FTE = 40 hours per week) [Unpublished provisional data]
Health NZ Te Whatu Ora. (2025, April 14). Elective Services Patient Flow Indicators Web Tool. Retrieved 28/04/2025 https://tewhatuora.shinyapps.io/ESPI_app/
Newshub. Quinn, R. (2020, April 28). Coronavirus: Hundred could die of cancer if hospitals don't catch up after lockdown - Cancer Society. Retrieved 22/05/2024 https://www.newshub.co.nz/home/new-zealand/2020/04/coronavirus-hundred-could-die-of-cancer-if-hospitals-don-t-catch-up-after-lockdown-cancer-society.html
Newsroom. Williams, D. (2021, Dec. 29). The tragedy and triumph of charity hospitals. Retrieved 05/04/2023 https://www.newsroom.co.nz/the-tragedy-and-triumph-of-charity-hospitals
NZ Doctor. Forbes, S. (2024, March 18). Te Whatu Ora still battling surgery waitlist challenge. Retrieved 22/05/2024 https://www.nzdoctor.co.nz/article/news/te-whatu-ora-still-battling-surgery-waitlist-challenge
NZ Herald. Russell, E. (2019, Oct.11). Blair Vining fought tirelessly to fix how we treat cancer. He just lost his own battle with the disease. Retrieved 22/04/2023 https://www.nzherald.co.nz/nz/blair-vining-fought-tirelessly-to-fix-how-we-treat-cancer-he-just-lost-his-own-battle-with-the-disease/ONZYFLCRRNTOUCX4N7YLZMVXIU/#:~:text=Vining%20was%20diagnosed%20with%20terminal,when%20he%20was%20just%2038
NZ Herald. Davison, I. (2023, Sept. 29). The places in New Zealand where patients are 100km from a doctor. Retrieved 22/05/2024 https://www.nzherald.co.nz/nz/the-places-in-new-zealand-where-patients-are-100km-from-a-doctor/LWQYEFAUXJG73OZGZQA5RRQVFY/
NZ Herald. Jones, N., and Preston, N. (2020, May 4). Covid-19 coronavirus: Elective surgeries ramping up after 30,000 operations delayed due to lockdown. Retrieved 22/05/2024 https://www.nzherald.co.nz/nz/covid-19-coronavirus-elective-surgeries-ramping-up-after-30000-operations-delayed-due-to-lockdown/PVBHKES3LWGZVHVXTSCHFGIT5A/
NZ Herald. Russell, E., and Gabel, J. (2022, May 4). Hospital waiting lists: Health Minister Andrew Little airs plan to tackle growing delays. Retrieved n.d. https://www.nzherald.co.nz/nz/hospital-waiting-lists-health-minister-andrew-little-airs-plan-to-tackle-growing-delays/YUDQOKCJPAVGLT2D2UMGDIZ5ME/
Pressreader NZ. The Press. Lewis, O. (2019, Dec. 31). Poor fall through the cracks. Retrieved 31/12/2019 https://www.pressreader.com/new-zealand/the-press/20191231/281569472646242
RNZ. Hill, R. (2024, May 13). Health funding fails to keep up with inflation or demand - doctors’ union. Retrieved 22/05/2024 https://www.rnz.co.nz/news/political/516635/heath-funding-fails-to-keep-up-with-inflation-or-demand-doctors-union
RNZ. Crimp, L. (2024, March 1). Up to 400 waiting more than a year for surgery despite target of zero. Retrieved 22/05/2024 https://www.rnz.co.nz/news/national/510599/up-to-400-waiting-more-than-a-year-for-surgery-despite-target-of-zero
RNZ. (2023, Oct. 31). Number of patients waiting over four months to see a specialist jumps 46% in last year. Retrieved 22/05/2024 https://www.rnz.co.nz/news/national/501389/number-of-patients-waiting-over-four-months-to-see-specialist-jumps-46-percent-in-last-year
RNZ. Chittock, N. (2022, May 6). Hospital waiting lists: Painful wait for surgery pre-dates Covid-19, sufferers say. Retrieved 22/05/2024 https://www.rnz.co.nz/news/national/466533/hospital-waiting-lists-painful-wait-for-surgery-pre-dates-covid-19-sufferers-say
RNZ. Pennington, P. (2024, April 19). Union dismay over Te Whatu Ora hospital staffing limits to trim budget deficits. Retrieved 22/05/2024 https://www.rnz.co.nz/news/national/514722/union-dismay-over-te-whatu-ora-hospital-staffing-limits-to-trim-budget-deficits
RNZ. Hanafin, G. (2024, May 10). Nurses protest, warn patients being left in pain, soiled beds due to staffing shortages. Retrieved 22/05/2024 https://www.rnz.co.nz/news/national/516439/nurses-protest-warn-patients-being-left-in-pain-soiled-beds-due-to-staffing-shortages
Scoop Independent News. (2024, Feb. 15). Hospital Infrastructure Deficit Shows A Different Path Is Needed. Retrieved 22/05/2024 https://www.scoop.co.nz/stories/PO2402/S00091/hospital-infrastructure-deficit-shows-a-different-path-is-needed.htm
Southern Charity Hospital. Retrieved n.d. https://www.southlandcharityhospital.org/
Stats NZ. (2022). One million people aged 65+ by 2028. Retrieved 17/08/2023 https://www.stats.govt.nz/news/one-million-people-aged-65-by-2028/
Stuff. Savory, L. (2019). Cancer advocate Blair Vining celebrated at memorial service. Retrieved 06/04/2024 https://www.stuff.co.nz/national/116585583/cancer-advocate-blair-vining-celebrated-at-memorial-service
Stuff. Newman, T. (2019, Sept. 7). National Portrait: Blair Vining - campaigning against cancer. Retrieved n.d https://www.stuff.co.nz/national/health/115516240/national-portrait-blair-vining--campaigning-against-cancer
Stuff. Rankin, J. (2021, Nov. 27). Painful waits for surgery grow longer for MidCentral Health patients. Retrieved 06/04/2023 https://www.stuff.co.nz/national/health/127107099/painful-waits-for-surgery-grow-longer-for-midcentral-health-patients?rm=a\
Stuff. Steyl, L. (2022, Oct. 21). More than 10,000 people on Southern hospital wait lists. Retrieved 05/04/2023. https://www.stuff.co.nz/national/health/130244453/more-than-10000-people-on-southern-hospital-wait-lists
Stuff. Moore, R. (2022, Nov. 7). 20,000 people wait for surgery or first look in Waikato. Retrieved 08/04/2023 https://www.stuff.co.nz/national/health/300730762/20000-people-wait-for-surgery-or-first-look-in-waikato
Stuff. Forbes, S. (2022, Dec. 24). Elective surgery waiting list numbers up 53% in Counties Manukau. Retrieved 06/04/2023 https://www.stuff.co.nz/national/politics/local-democracy-reporting/300773056/elective-surgery-waiting-list-numbers-up-53-in-counties-manukau?rm=a
Stuff. Martin, H. (2023, Sept. 8). Thousands waiting more than a year for planned medical treatment. Retrieved 22/05/2024 https://www.stuff.co.nz/national/health/300950265/thousands-waiting-more-than-a-year-for-planned-medical-treatment
Stuff. Steyl, L. (2024, Jan. 8). Long wait lists result of ageing population, health boss says. Retrieved 22/05/2024 https://www.stuff.co.nz/national/health/133533653/long-wait-lists-result-of-ageing-population-health-boss-says
Te Kāwanatanga o Aotearoa New Zealand Government. (2021). Seeing a specialist. Retrieved 20/04/2023. https://www.govt.nz/browse/health/gps-and-prescriptions/seeing-a-specialist/#:~:text=If%20the%20medical%20specialist%20decides,is%20up%20to%204%20months.
Te Tūāpapa Kura Kāinga - Ministry Of Housing And Urban Development. (2023, March 30).The long-term implications of our ageing population for our housing and urban futures. Retrieved 22/05/2024 https://www.hud.govt.nz/news/the-long-term-implications-of-our-ageing-population-for-our-housing-and-urban-futures
The Conversation. Gauld, R. (2023, Feb. 7). NZ’s health system has been under pressure for decades. Reforms need to think big and long-term to be effective. Retrieved 22/05/2024 https://theconversation.com/nzs-health-system-has-been-under-pressure-for-decades-reforms-need-to-think-big-and-long-term-to-be-effective-198495
ON THIS PAGE
Download our insurance comparison chart
We need a few details before we can send you this content…
* All fields are required

